What Is Abnormal Uterine Bleeding?
Abnormal uterine bleeding refers to any bleeding from the uterus that differs from your normal menstrual cycle. This includes:
• Bleeding between periods.
• Heavy or prolonged periods (menorrhagia).
• Irregular periods.
• Bleeding after menopause.
• Spotting or bleeding after intercourse.
While occasional irregularities in menstrual cycles can be normal, persistent or severe changes warrant medical attention.
Common Causes of Abnormal Uterine Bleeding
Hormonal Imbalances
• Anovulation: When the ovaries fail to release an egg, hormone levels become unbalanced, leading to irregular or heavy bleeding.
• Polycystic Ovary Syndrome (PCOS): A hormonal disorder that disrupts ovulation and menstrual cycles.
• Thyroid Disorders: Both hypothyroidism and hyperthyroidism can affect menstrual patterns.
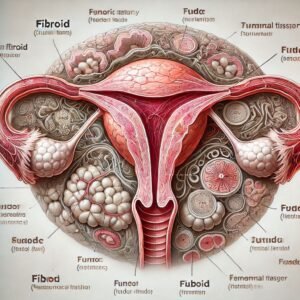
Structural Abnormalities
• Fibroids: Noncancerous growths in the uterus that can cause heavy bleeding or prolonged periods.
• Polyps: Small, benign growths in the uterine lining that may lead to spotting or irregular bleeding.
• Adenomyosis: A condition where the uterine lining grows into the muscular wall, causing heavy and painful periods.
Medical Conditions
• Bleeding Disorders: Conditions like von Willebrand disease can lead to excessive menstrual bleeding.
• Pelvic Infections: Infections of the reproductive tract, such as pelvic inflammatory disease (PID), can result in abnormal bleeding.
• Endometrial Hyperplasia: Thickening of the uterine lining, sometimes a precursor to cancer.
• Endometrial or Cervical Cancer: Rare but serious causes of postmenopausal or abnormal bleeding.
Medications and Lifestyle Factors
• Hormonal Contraceptives: Birth control pills, intrauterine devices (IUDs), or hormone therapy can sometimes cause irregular bleeding.
• Blood Thinners: Medications like aspirin or anticoagulants may contribute to heavier bleeding.
• Stress and Lifestyle Changes: Stress, significant weight changes, or excessive exercise can disrupt menstrual cycles.
Diagnosing Abnormal Uterine Bleeding
If you experience abnormal bleeding, your healthcare provider will perform a thorough evaluation, which may include:
1. Medical History: Discussing your symptoms, menstrual patterns, and any underlying conditions.
2. Physical Exam: Including a pelvic exam to assess for signs of infection or abnormalities.
3. Blood Tests: To check for anemia, thyroid function, or clotting disorders.
4. Imaging Tests: Ultrasound, hysteroscopy, or MRI to visualize the uterus and identify structural issues.
5. Endometrial Biopsy: A sample of the uterine lining may be taken to rule out cancer or other conditions.